Inflammatory Bowel Disease (IBD): Symptoms, Causes and Treatment

Dr Tan Wah Siew
Senior Consultant Colorectal Surgeon
MBBS (Singapore), MMed (Surgery), FAMS, FRCS
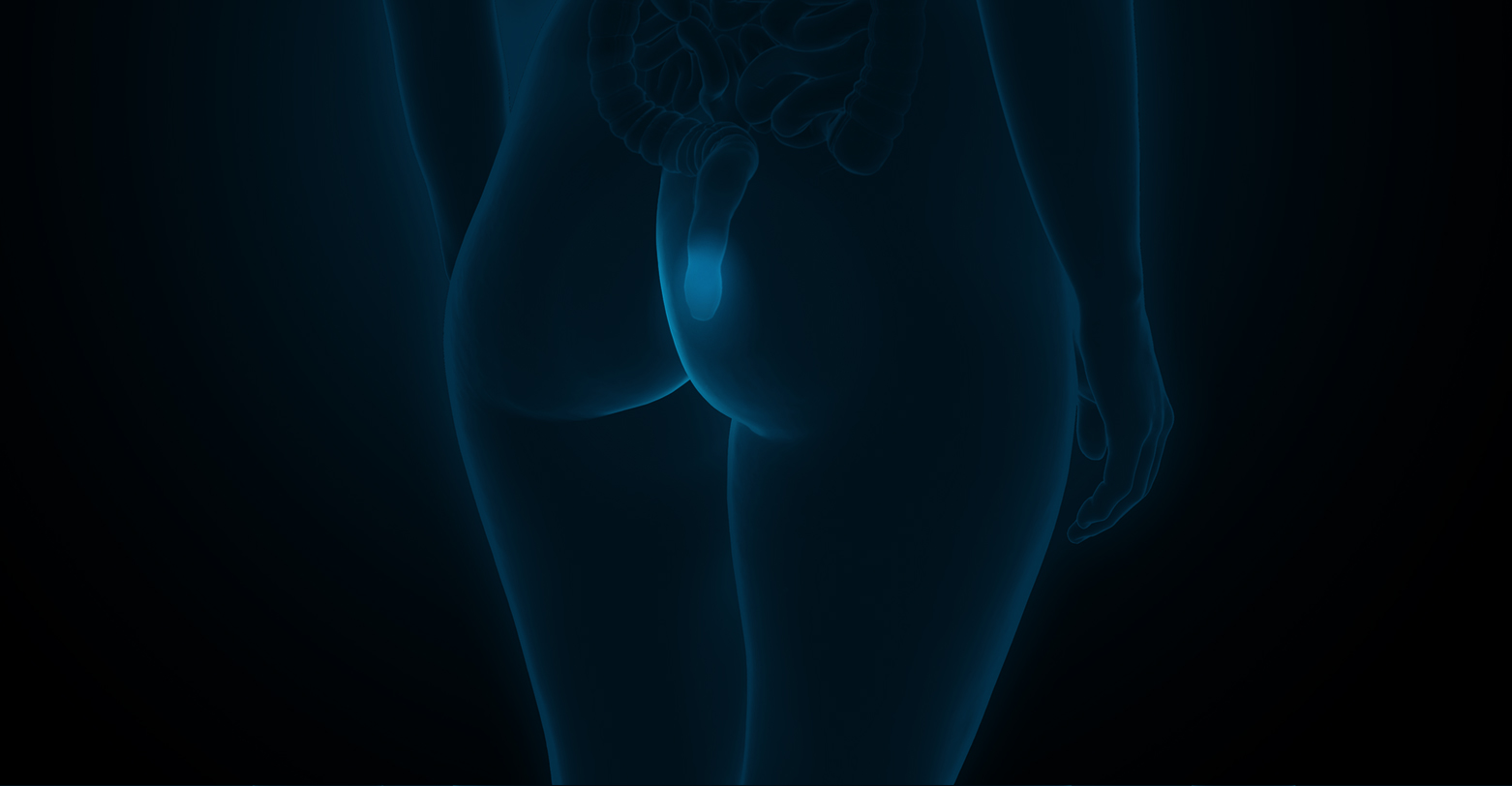
IBD is an umbrella term for conditions where the digestive tract becomes persistently inflamed. This ongoing inflammation can affect different sections of your intestines, leading to a wide range of symptoms that vary in intensity from person to person. Because it is a chronic condition, IBD requires careful management, but with the right support, you can maintain your well-being and continue with your daily activities.
Ulcerative colitis primarily affects the colon and rectum, causing inflammation and small sores, known as ulcers, in the lining of the bowel. The inflammation usually starts in the rectum and can spread through the colon to varying degrees. Symptoms may include frequent diarrhoea, sometimes with blood, abdominal discomfort and fatigue. Because ulcerative colitis affects only the innermost lining of the bowel, treatment often focuses on controlling inflammation and maintaining remission.
Crohn’s disease can affect any part of the digestive tract, from the mouth to the anus, though it most commonly involves the small intestine and colon. Unlike ulcerative colitis, Crohn’s can involve all layers of the bowel wall, which can lead to complications such as narrowing of the intestines or fistula formation. Symptoms may vary widely depending on the area affected, but often include abdominal pain, weight loss, diarrhoea and fatigue.
The symptoms of IBD can depend on which part of the digestive tract is affected and how severe the inflammation is. Common signs include:
Some people may also experience inflammation in other parts of the body, such as the joints, eyes, bile ducts, lungs or skin.
The exact cause of IBD is not fully understood, but research suggests it develops from a combination of genetic, environmental and immune factors. While the triggers can vary between individuals, several elements are known to increase the risk of developing the condition:
If left unmanaged, IBD can lead to a range of complications, some of which can be serious:
Confirming a diagnosis of IBD usually involves a combination of tests, as doctors aim to rule out other causes of your symptoms:
Living with IBD requires ongoing care and lifestyle changes to keep symptoms manageable and prevent flare-ups. These include:
Inflammatory bowel disease requires timely medical care to prevent symptom progression and reduce long-term complications. At Surgical Associates, care focuses on thorough evaluation, personalised treatment plans and nutritional guidance to support daily comfort and quality of life. Our IBD specialist, Dr Tan Wah Siew, provides assessment and ongoing management tailored to each patient’s condition. If you have IBD or suspect you may be affected, book a consultation for a detailed evaluation and to discuss treatment options suited to your needs.
IBD is a chronic condition and cannot currently be cured. However, with appropriate medical treatment, lifestyle adjustments and, in some cases, surgery, many people achieve long periods of remission.
IBD develops due to a combination of genetic, immune and environmental factors. While the exact triggers vary between individuals, infections, certain medications, diet and stress may contribute to symptom flare-ups.
Yes, IBD can occur in children, including both Crohn’s disease and ulcerative colitis. Early diagnosis and treatment are important to manage symptoms, support normal growth and reduce the risk of complications.
Yes, IBD can usually be managed safely during pregnancy and breastfeeding. Many medications are considered safe, but treatment should always be reviewed by a specialist.
IBD is a chronic inflammatory condition that causes ongoing inflammation and tissue damage in the intestines. IBS, or irritable bowel syndrome, is a functional bowel disorder that does not cause inflammation or permanent damage.

MBBS (Singapore), MMed (Surgery)
Fellow of the Academy of Medicine Singapore
Fellow of the Royal College of Surgeons of Edinburgh
Dr Tan Wah Siew is a senior consultant colorectal surgeon with experience managing a wide range of colorectal conditions, including inflammatory bowel disease. She has been part of the multidisciplinary IBD team at Singapore General Hospital since 2016, working closely with gastroenterologists and other specialists to guide care decisions. When surgery is required for ulcerative colitis or Crohn’s disease, Dr Tan adopts an approach tailored to the individual patient, selecting surgical techniques based on disease severity, overall health and recovery considerations.


Mount Elizabeth Medical Centre
#08-07, 3 Mount Elizabeth, Singapore 228510
Tel: 6454 0054
|
Fax: 6764 0054
|
Email: ask@surgicalassociates.sg
Gleneagles Medical Centre
#05-01, 6 Napier Road, Singapore 258499
Tel: 6471 0054
|
Fax: 6271 0054
Need medical advice from Dr Lee or Dr Tan? Leave us a message and we will attend to you within one working day.